Image credit: Pexels
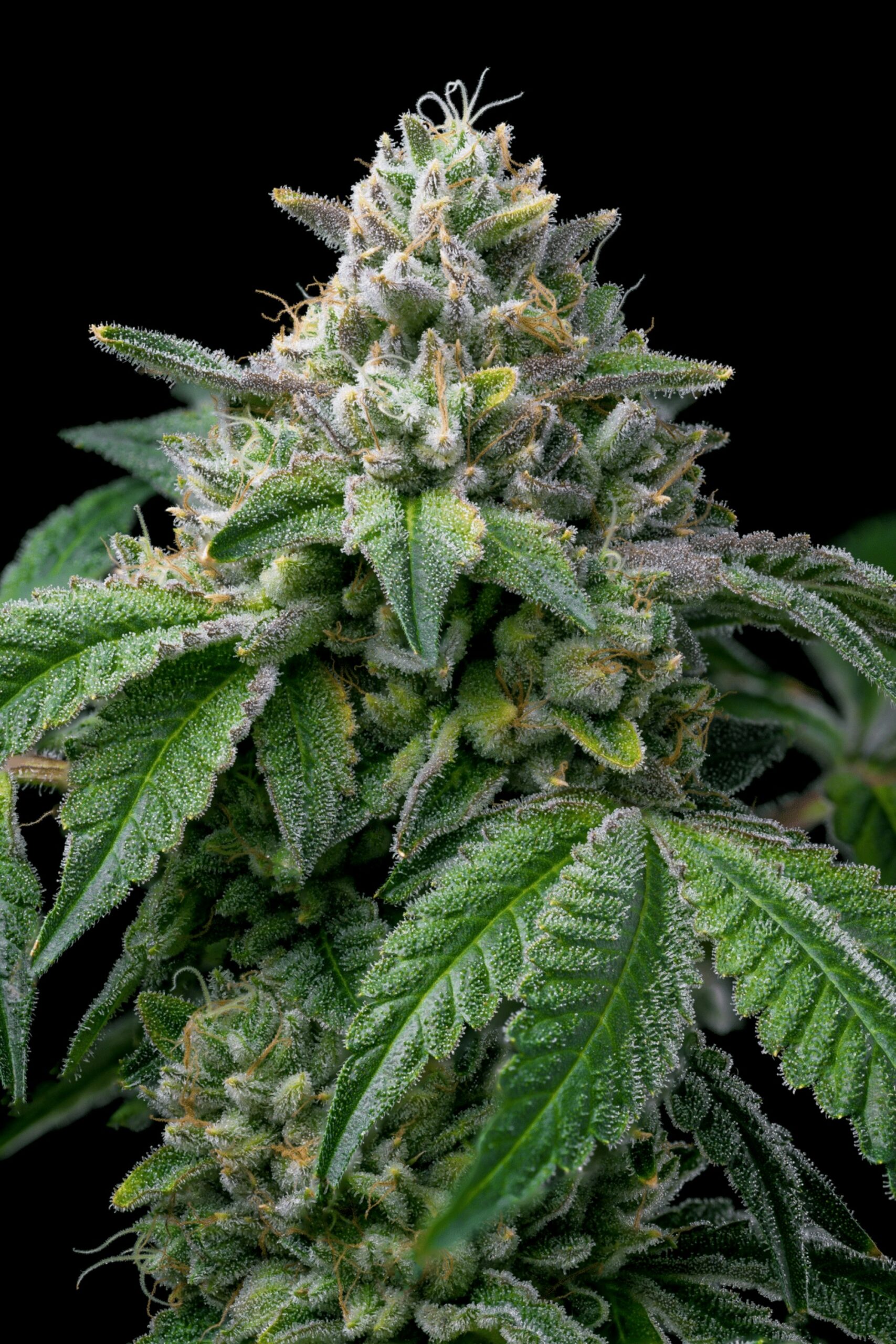
According to recent studies, the cannabis industry is ever-evolving, and so is the understanding of marijuana’s impact. A team of dedicated researchers from SUNY Upstate Medical University in Syracuse have unveiled findings that challenge conventional assumptions about the relationship between marijuana use and cognitive decline. The groundbreaking study, recently published in the esteemed journal Current Alzheimer Research, honed in on respondents aged 45 years and older in Washington DC and 14 U.S. states.
Departing from prior research that linked cognitive decline to the later development of dementia, the study introduces a new perspective. It reveals a “significant” association between recreational cannabis use and reduced odds of subjective cognitive decline (SCD). Notably, non-medical cannabis use arises as a standout, exhibiting a remarkable 96% decreased odds of SCD when compared to non-users. Even individuals who use marijuana for medical purposes or a combination of medical and recreational purposes displayed decreased odds of SCD, though not reaching statistical significance.
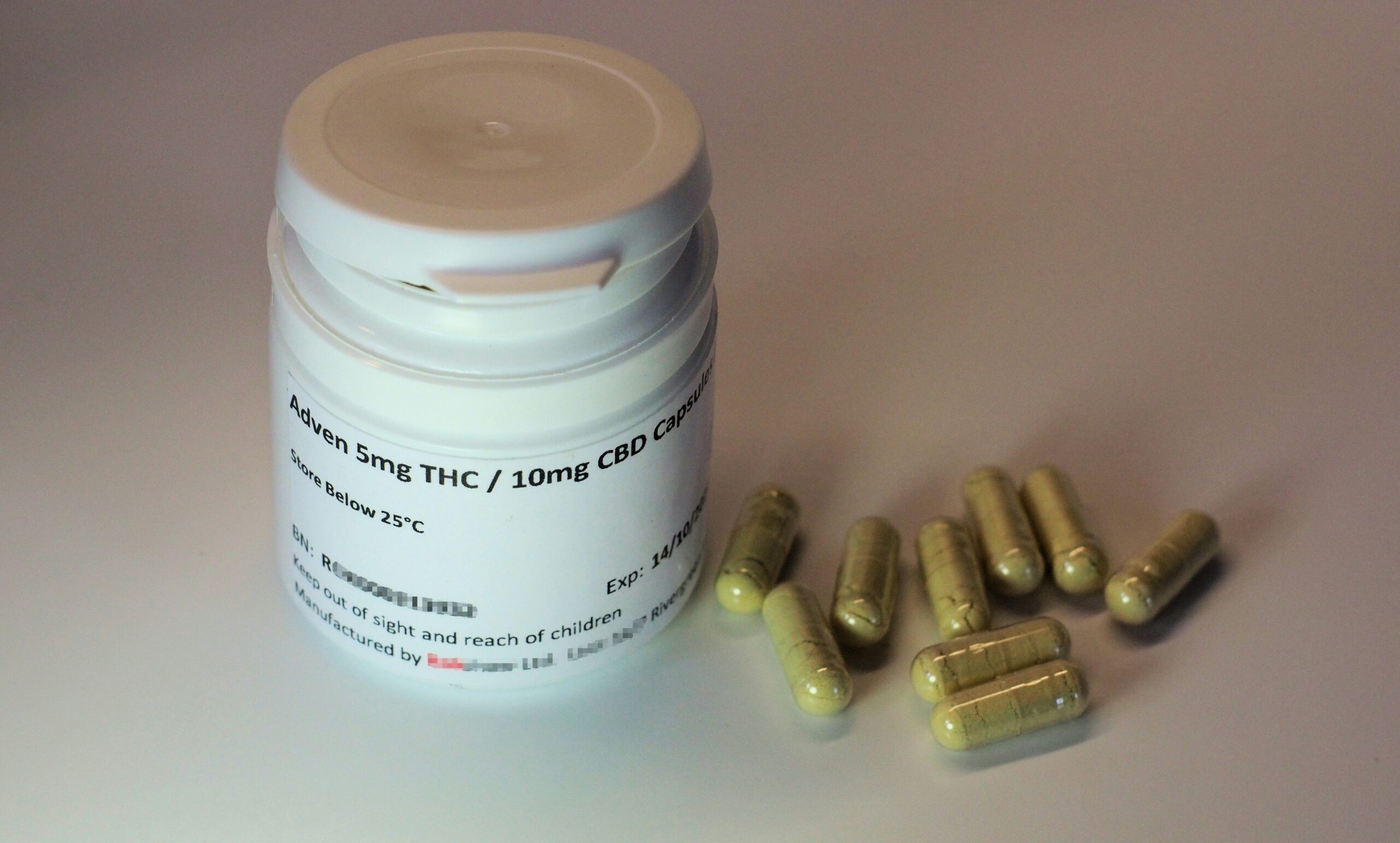
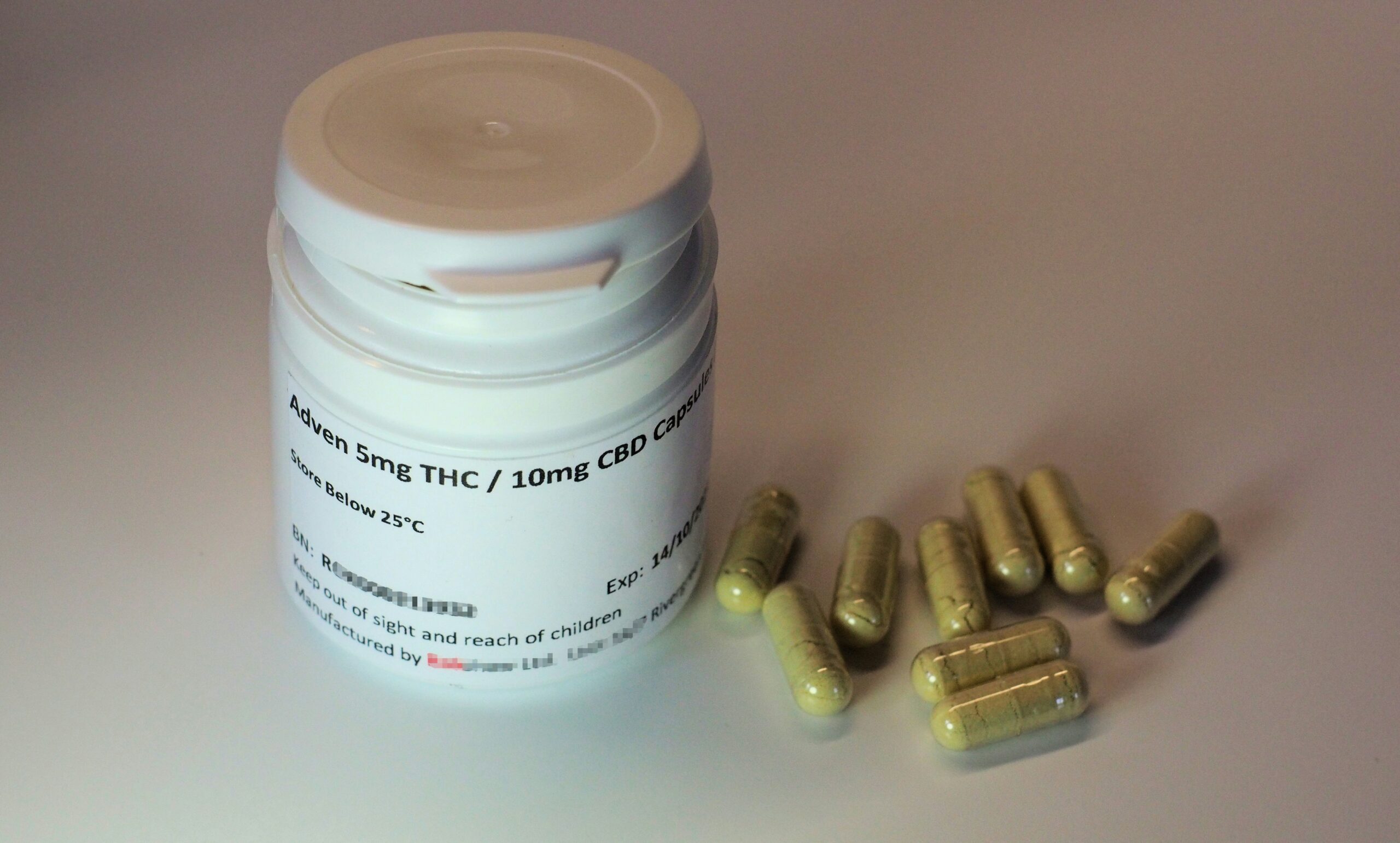
The study delved into various cannabis variables, scrutinizing the frequency of use, reasons for use, and methods of consumption. It boldly challenges the simplistic notion that the cognitive implications of cannabis use are solely determined by consumption frequency. Instead, the researchers suggest that factors like product formulation, method of administration, and reasons for use play crucial roles in shaping the cognitive effects associated with cannabis use.
While certain tests indicated a positive association between cannabis use frequency and SCD, these relationships were not deemed statistically significant. The method of cannabis use also produced mixed results, with a higher prevalence of SCD observed among cannabis smokers. The study commendably recognizes these complexities, emphasizing the need for a nuanced understanding of the multifaceted relationship between cannabis use and cognitive decline.
Exploring potential reasons for the observed decrease in SCD among cannabis users, the study puts forth several intriguing theories. One notable explanation revolves around the connection between cannabis use and improved sleep quality. Individuals often turn to marijuana to address issues such as insomnia and sleep disturbances, which are themselves associated with a heightened risk of dementia. By contributing to better sleep quality, cannabis use could indirectly serve to reduce the risk of cognitive decline.
The study also thoughtfully highlights the potential stress-relieving effects of cannabis, particularly through the use of CBD, a prominent component of cannabis. Stress reduction holds significant weight, especially considering that elevated stress levels are consistently linked to reduced cognitive function in older adults. The researchers further support their theories by referencing a 2017 mice study that indicated very low doses of THC, another component of cannabis, could potentially improve cognitive impairment in older females.
While this study contributes valuable insights to the growing body of knowledge surrounding marijuana, it diligently acknowledges certain limitations. The potential for response bias, especially from states where non-medical cannabis use remains illegal, and the self-reported nature of the data are recognized as constraints. Additionally, the study did not explore possible differences by geographic location, an aspect that warrants further investigation.
Ultimately, the research adds a fresh and nuanced layer to the evolving discourse on marijuana, particularly as more jurisdictions express considerations toward ending prohibition. The relationship between cannabis use and cognitive decline remains intricate and context-dependent across diverse demographics as comprehensive studies continue to shed new light.