Image credit: Unsplash
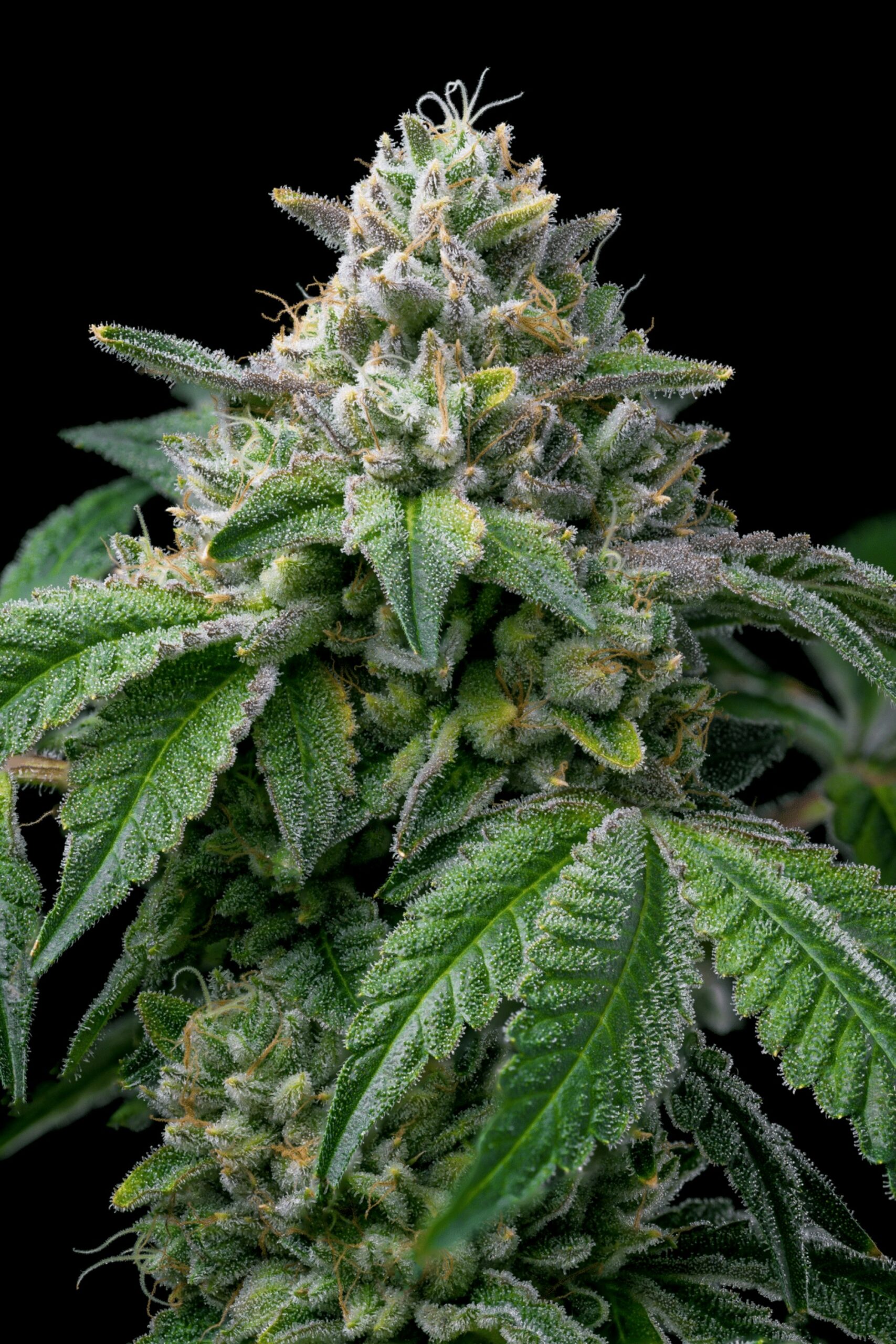
Researchers at Washington University in St. Louis have found that adolescents who use cannabis regularly report more psychotic spectrum symptoms and greater distress as a result of them, suggesting that a shared vulnerability and self-medication can contribute to the association between cannabis use and psychosis risk.
Associations with psychosis
The use of cannabis among adolescents has become associated with a higher risk of psychosis, with most users being two to four times more likely to develop psychosis symptoms than non-users. Early initiation during a child’s adolescence is linked to earlier onset of psychotic disorders, more severe symptoms, and a greater likelihood of symptom relapse.
Among adolescents, cannabis is the most frequently used illicit substance, with usage increasing from 11% to 22% over the last two decades, based on a source cited within the study. A perceived risk of harm associated with cannabis has decreased among adolescents, dropping to 36.3% to 25%, considering weekly use as being problematic.
A debate continues surrounding the nature of the association between the use of cannabis during adolescence and psychosis risk. Theories associated with this include the contributing risk hypothesis, the shared vulnerability hypothesis, and the self-medication hypothesis.
The varied hypotheses
In the contributing risk hypothesis, the use of cannabis causes the emergence and progression of psychosis symptoms through the disruption of the neurodevelopmental processes during a child’s adolescence.
In the shared vulnerability hypothesis, the genetic, gestational, or environmental factors predispose individuals to cannabis use as well as psychosis. In these scenarios, the likelihood of engaging with cannabis use shares similar origins as the risk of psychosis spectrum symptoms.
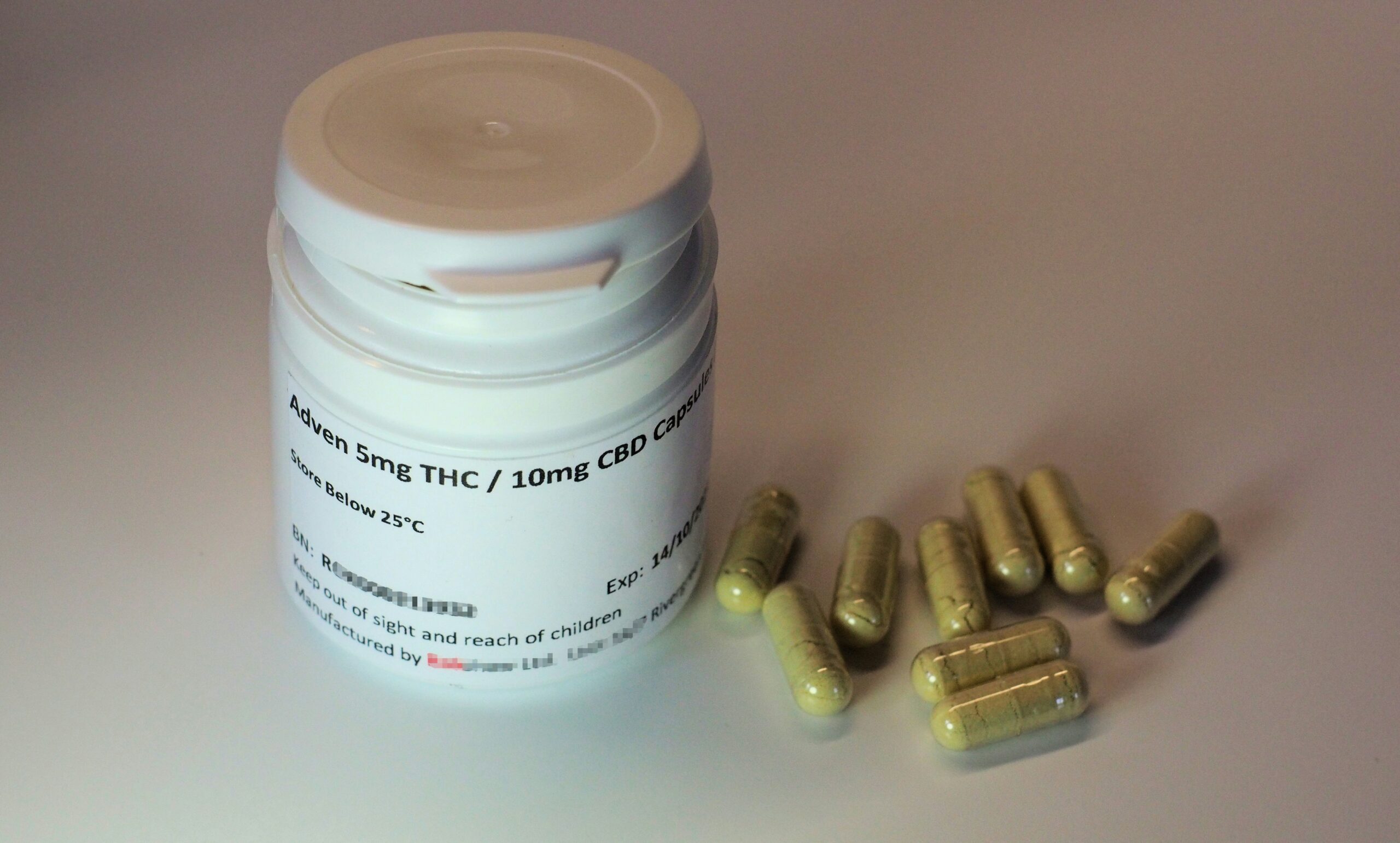
The self-medication hypothesis suggests that individuals may turn to cannabis to alleviate distressing symptoms that are associated with the psychosis spectrum.
Previous research has offered evidence supporting each model, but there continues to be a lack of prospective longitudinal studies focusing on early adolescence.
The ABCD Study
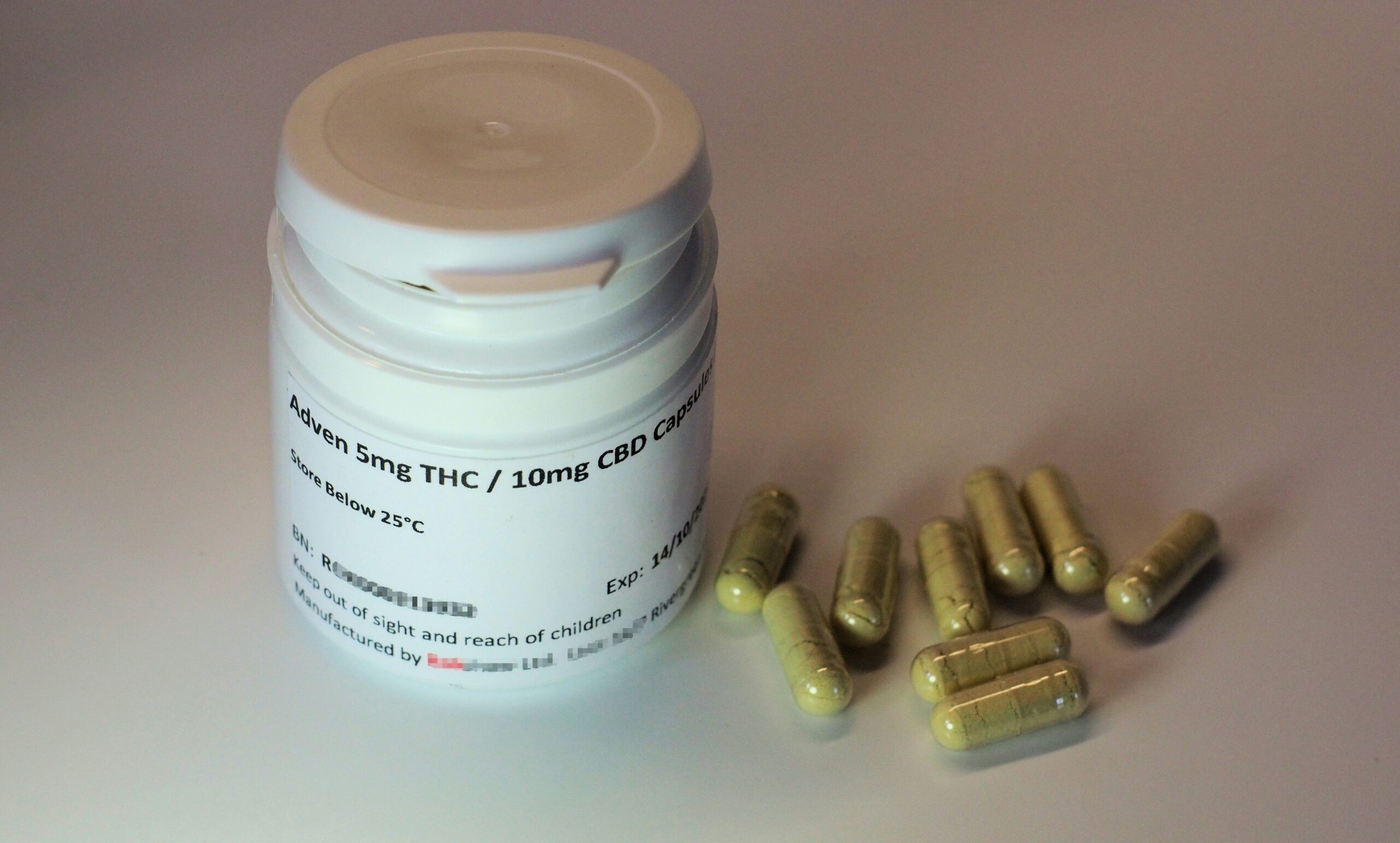
In the study “Psychosis Spectrum Symptoms Before and After Adolescent Cannabis Use Initiation,” which was published online in JAMA Psychiatry, researchers analyzed psychosis spectrum symptom trajectories before and after the initiation of cannabis in 11,868 adolescents from the ages of 9 to 10 years at baseline using the data from five ways over four years from the Adolescent Brain Cognitive Development (ABCD) Study.
Cannabis initiation did not consistently lead to an increase in psychosis symptoms, providing no significant support for the contributing risk hypothesis.
Meanwhile, adolescents who used cannabis at any point during the study period reported greater numbers of psychosis spectrum symptoms and were more distressed compared to others who had never used cannabis, supporting the shared vulnerability hypothesis.
An increase in the number of psychosis spectrum symptoms, as well as the associated distress leading up to cannabis initiation, was observed before cannabis use began, which aligned well with the self-medication hypothesis.
Based on the findings observed, the current research supports the shared vulnerability and self-medication explanation for associations between cannabis use and the risk of psychosis.
Past studies on the influence of brain inflammation
In past studies, researchers at Washington University have discovered that there are biological clues that show connections between cannabis exposure in the womb and adolescent behavioral problems. Sarah Paul and David Baranger, in the Behavioral Research and Imagiging Neurogenetics (BRAIN) lab, led by Ryan Bodgan, have found associations between prenatal cannabis exposure and potential mental health problems that persisted in childhood and adolescence.
“We see evidence that cannabis exposure may influence the developing brain, consistent with associations with mental health,” Baranger said.
During their studies, researchers looked at a variety of neuroimaging measurements that factor into brain development, which include brain thickness and surface area, as well as the measures that reflect water diffusion in and outside of cells. The patterns revealed in the group exposed to cannabis have been consistent with potential reductions in neuroinflammation. However, researchers have also pointed out that reduction of inflammation at the wrong times can affect how the brain is “pruned and primed.”